Hip Surgery
 About Hip Replacement Surgery
About Hip Replacement Surgery
Over time, the impact of joint injury, arthritis, or excessive body weight can erode the hip joint. Arthritis can be an inherited disease process that appears with age. One risk factor that is under the control of the person is their body weight. Excessive body weight can wear out the normal knee and hip joints which were never intended to carry a human that is morbidly obese.
The problem of obesity is growing, which in turn causes more joint problems. As of 2015, 34.9% of U.S. adults are obese or morbidly obese, according to the Journal of American Medicine (JAMA). The study also found that obesity worsens as a person enters their 40s and 50s. Obesity is higher among middle age adults, 40-59 years old (39.5%) than among younger adults, age 20-39 (30.3%) or adults over 60 or above (35.4%) adults.
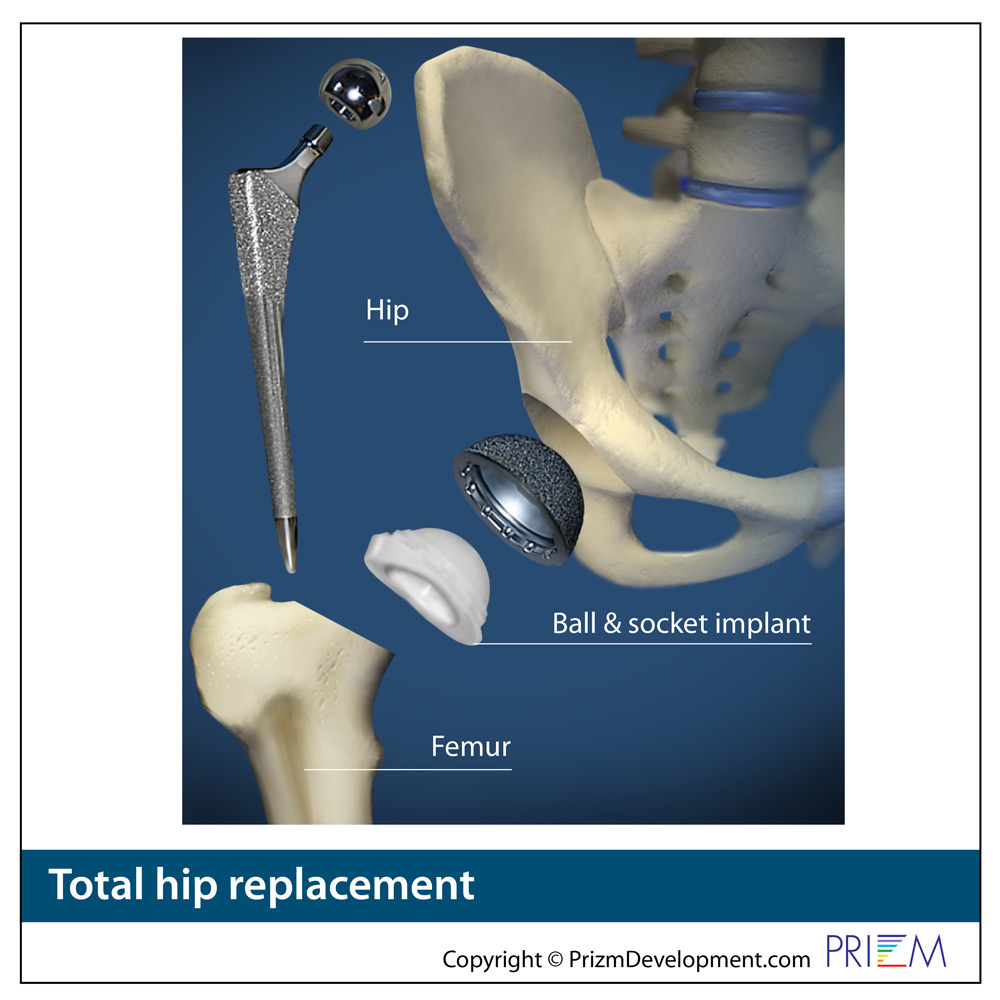
Artificial hip joints
According to the American Academy of Orthopaedic Surgeons, each year in the United States, about 193,000 hip replacements are performed. With the aging of the post-World War II baby boom generation (those born between 1946-1964), that number is expected to grow significantly as this large segment of the population now age into their 50s, 60s and 70s. It is estimated that more than 500,000 knee and hip replacements will be done each year by 2040.
Also, the joint implant technology involved is improving, enabling the artificial joint to last longer. This enables more surgeons to recommend hip replacement with the belief that the artificial hip joint may outlive the life of the patient, thereby eliminating the need for a revision surgery on an elderly patient in their 70s or 80s.
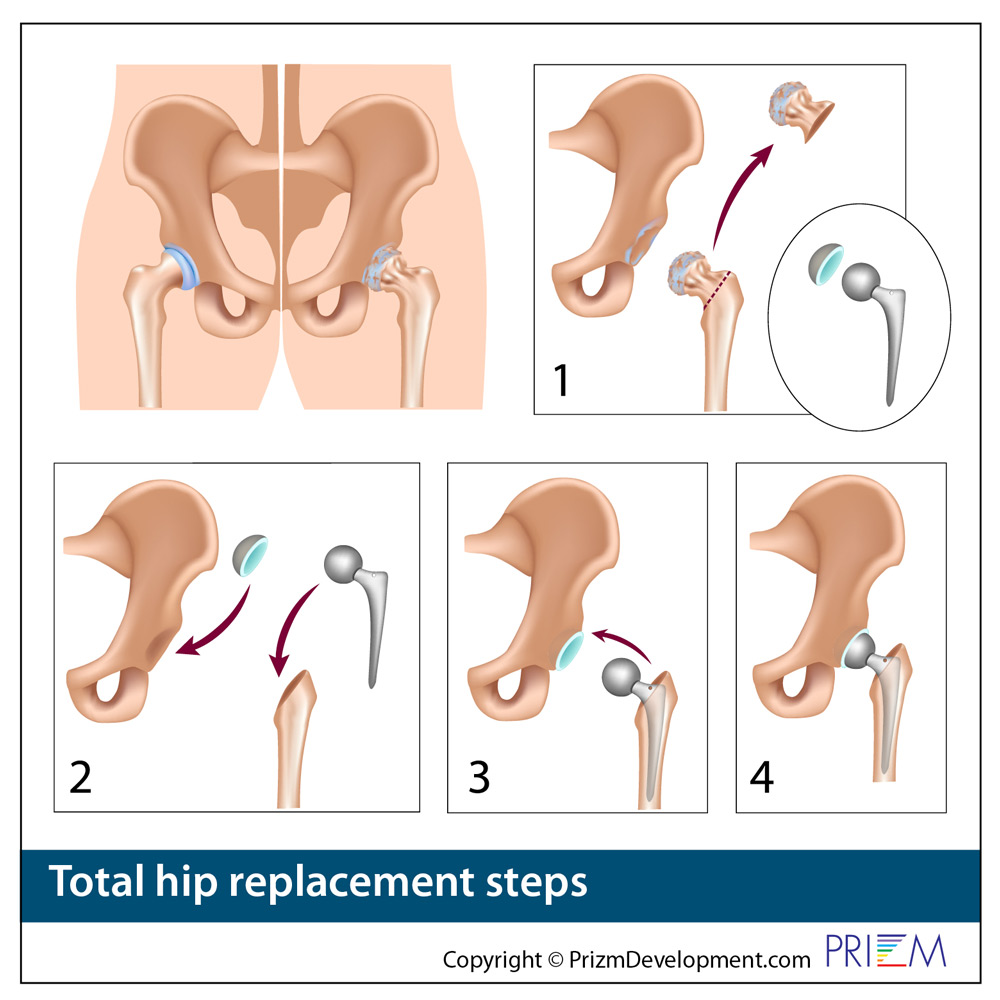
Traditional open hip replacement surgery lasts between one-to-two hours, although an extremely proficient hip surgeon who does a large volume of cases may be faster. The hip surgeon makes an incision along the side of the hip and carefully moves the muscles at the top of the thighbone to reveal the hip joint. The surgeon then removes the ball and socket portions of the joint. Artificial joint parts are inserted into the thighbone and pelvis, and fixed into position to create the artificial joint.
Traditional open hip replacement surgery typically requires an incision about 5 to 8 inches in length. Through the incision, muscles and tissues are separated and the hip joint is exposed for hip replacement. The surgeon removes the arthritic hip joint and replaces the arthritic hip with the artificial hip joint implant. The surgeon performs this surgery by looking directly at the arthritic hip joint and setting the artificial hip implant into place. After traditional hip replacement surgery, patients may stay in the hospital for four or five days and can require several months of rehab and therapy to regain pain free movement.
Through Minimally Invasive Hip Replacement, the hip surgeon performs the same hip replacement surgery through two small incisions. The surgeon does not look directly at the arthritic hip, but uses X-ray guidance in the operating room to position the artificial hip. Patients who undergo minimally invasive hip replacement surgery have a shorter one or two day stay in the hospital, smaller scar around the hip joint, less disruption to the hip muscles, a faster rehab and less painful recovery period.
Minimally invasive hip replacement surgery is still new and some surgeons believe relying on X-rays for positioning of the implant can be less precise than working with a larger open hip joint incision.
Not all patients qualify for minimally invasive hip replacement surgery. Your joint replacement surgeon will be able to explain in more detail the pros and cons of minimally invasive hip replacement surgery and if you qualify.
The life of the artificial joint
Historically, artificial hip joints may wear out after 15 to 20 years, and outcomes of revisions are less ideal than original hip replacements. Consequently, surgeons try to delay hip replacement surgery as long as possible. In the United States, 65 percent of hip replacements are performed on those patients over the age of 65. It is also not recommended for the extremely obese, those with a terminal illness, on renal dialysis, or those with nerve disease. With newer materials that are now available, the expectation is a lifespan of up to 30 years.
The pros and cons of anterior vs. posterior hip replacement surgery
About 70 percent of hip replacement surgeries today are performed through a traditional posterior approach through the buttock area. Most medical schools train orthopedic surgeons to use the traditional posterior approach as the primary approach.
Some hip surgeons favor an alternative approach from the anterior side, or front side of the hip.
Direct anterior hip replacement
Direct Anterior Hip Replacement is a new surgery method that is an alternative to the conventional hip replacement surgery and is growing in popularity. It's currently only used in about 20% of cases in the U.S. In the past, hip replacement surgery required cutting certain muscles and tendons in order to access the area being fixed. Conversely, direct anterior hip replacement does not require the cutting of muscles or tendons to expose the joint being treated. This new surgery can be more difficult and requires special equipment including surgical instruments and operating tables.
Some studies have shown that Direct Anterior Hip Replacement surgery patients may have a faster recovery and may have less post-operative pain and discomfort than traditional hip replacement surgery. A 2014 study of 54 patients found that anterior hip replacement patients were able to walk unaided 6 days earlier than other hip replacement patients. Other studies have shown that the Direct Anterior Hip Replacement has fewer dislocations.
Direct Anterior Hip Replacement surgery, however, is not for all candidates. Some hip surgeons feel that anterior hip replacement has some issues: The nerve which supplies sensation to the front and side of the thigh can be more vulnerable to injury during surgery. Those patients who are obese, short, or the person with very muscular thighs are more challenging with an anterior approach.
In conclusion, there can be disagreement among hip surgeons as to what approach is the best one for a specific patient, and it's important to listen to your surgeon's recommendation rather than try to shop for an approach that may not be appropriate for you.
Ceramic vs Plastic
There are a large number of hip implant devices on the market and each manufacturer has different models composed of different materials. Currently the most popular implants are metal-on-plastic and ceramic-on-plastic.
There is no consensus in the orthopedic community regarding the single “best” bearing or material. The choice generally comes down to the patient's specific requirements and the surgeon's preference. Surgeons consider many variables when choosing one device over another, including his or her personal experience as well as tool and implantation method preferences.
Metal-on-Plastic
Metal-on-plastic (polyethylene) is the longest tried and tested bearing. The femoral head is constructed of metal (usually a cobalt chrome alloy) and the cup liner is made of a plastic called polyethylene.
Because of its durability and performance, Metal-on-Plastic has been the leading artificial hip component material chosen by surgeons since hip replacement surgeries have been performed.
Ceramic-on-Plastic
Ceramic is the 21st century answer to hip replacement as it is both hard and durable, it wears minimally and the material is widely deemed to have no toxic or side effects in the human body.
Ceramic-on-Plastic is a good combination of two very reliable materials. Ceramic heads are harder than metal and are the most scratch-resistant implant material. The hard, ultra-smooth surface can greatly reduce the wear rate on the polyethylene bearing. The potential wear rate for this type of implant is less than Metal-on-Polyethylene.
So why not choose ceramic-on-plastic every time? For one, ceramic heads are more expensive than metal. And in rare situations the ceramic head can shatter if the patient falls on their hip.
Only a qualified orthopedic surgeon can determine which implant system is best for your unique situation. There are many factors your surgeon uses when recommending hip implants. Be sure to ask questions and share any concerns you might have regarding specific implants with your surgeon early in the process.

The CORI Robotic Surgery System enhances the accuracy and safety of joint replacement surgery.
CORI ROBOTIC KNEE REPLACEMENT SURGERY
The CORI Robotic System enables orthopedic surgeon in performing joint replacement surgeries as in hip and knee joint replacement. The CORI robotics system uses 3-dimensional intraoperative software that enables the orthopedic surgeon to map out the joint replacement surgery with greater precision and install the artificial joint with much greater accuracy than the human eye.
The new robotic surgery systems provide the surgeon the power of the computer to precisely shape the joint space and place the artificial joint implant into the ideal position during surgery. The robotic technology not only improves the outcomes from joint replacement but also reduces the amount of time the patient is under anesthesia or imaging because the joint replacement surgery goes faster.
Mapping out the surgery in advance speeds the surgery the next day, as the robotic arms are preset precisely to a quarter of a millimeter that then enable the surgeon to more precisely install the artificial joint for the ideal fit. The CORI knee robotic system also controls the speed at which surgical screws or plates are installed creating the ideal speed of rotation.
While using robotic technology requires extensive training, the benefits for the patient are huge as surgery goes much faster. This means that the patient is spending less time under anesthesia and less time under fluoroscopy. The CORI robotic surgery system also often enables the orthopedic surgeon to operate through a smaller incision so the patient has less blood loss, less tissue disruption and less pain as they go through rehab and therapy. Some patients with robotic surgery go home later the same day rather than spending days in the hospital. Consequently, these patients are typically back to activity much faster than with traditional joint replacement surgery.

 Hip
Hip
 Hip
Hip