Osteoporosis
Osteoporosis and back pain
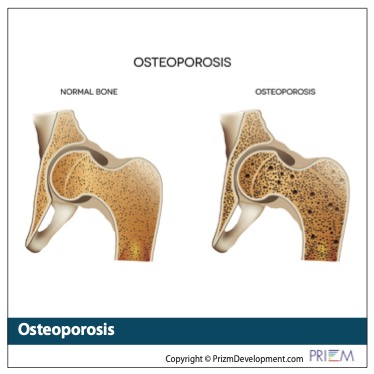
It's estimated that half of women over age 50 develop weakening of the bones, called osteoporosis, which can lead to painful back and neck pain symptoms.
The most common cause of osteoporosis pain is a spinal compression fracture. These fractures can be very painful because the collapsed vertebrae may pinch the nerves that radiate out from the spinal cord. The pain symptoms can range from minor tenderness to extreme back pain.
It can cause severe back pain that gets worse when standing or walking. Sometimes there is relief when you lie down and take the weight off your spine. Those with a compression fracture also experience extreme pain when twisting or bending the body.
What causes osteoporosis:
As you age, old bone tissue can break down faster than its created. This can cause your bones to become more porous and fragile. It can also result in severe back or neck pain.
The National Osteoporosis Foundation estimates that half of all women over the age of 50 will eventually develop osteoporosis and that 80 percent of Americans with osteoporosis are women. Women, the foundation reports, account for up to 80% of all hip fractures.
Risk factors for osteoporosis include:
• age over 50
• a woman going through menopause before age 45
• having ovaries removed before age 45
• having low estrogen in women
• men having low testosterone
• vitamin D deficiency
• smoking
• having a family history of osteoporosis
• not enough weight-bearing exercise
How is osteoporosis diagnosed?
Osteoporosis is diagnosed with a bone density diagnostic tool called dual energy X-ray absorptiometry (DXA), which scans your hip and spine to determine how dense your bones are compared to other people of your gender and age. White and Asian women, especially those past menopause, are at highest risk
While most people with osteoporosis are women, about 2 million are men.
Also, studies show that a first osteoporotic fracture makes it five times more likely further fractures will occur. This underscores why those with osteoporosis seek medical treatment with diet and medications to strengthen bone before it reaches the fracture stage.
How is osteoporosis treated?
The good news is that there are two procedures that treat osteoporosis and can relieve symptoms: Kyphoplasty and Vertebroplasty. Vertebroplasty and kyphoplasty are both minimally invasive surgical procedures for treating osteoporotic fractures where a cement-like material is injected directly into the fractured bone. This stabilizes the fracture and provides immediate pain relief in many cases.
Kyphoplasty
Kyphoplasty is a minimally invasive surgical treatment for fractures. Kyphoplasty involves using a small incision to insert a small balloon into the collapsed vertebrae to restore height and function to the spine. The balloon is replaced by cement that makes the bone strong again.
During a kyphoplasty, you will have medication through an IV to relax you. Using a C-arm that provides the spine specialist a view of your spine, a needle is inserted through your skin and guided into the spinal vertebra that is collapsed or fractured. A special balloon is inflated within the vertebra to enable the damaged vertebra to regain a normal shape. Using X-ray guidance, the spine physician then injects a special cement-like material into the reshaped vertebra which then hardens. The spine physician then removes the needle. No stitches are needed. The entire kyphoplasty procedure will probably usually takes less than an hour. If more than one vertebra is treated it may take slightly longer.
By restoring the vertebrae to a more normal state, alignment of the spine may be improved.
A pain prescription is typically provided to relieve any post-procedure soreness, and pain relief can follow within two days of surgery. Some patients report an immediate improvement in their pain symptoms when standing to walk immediately after the procedure.

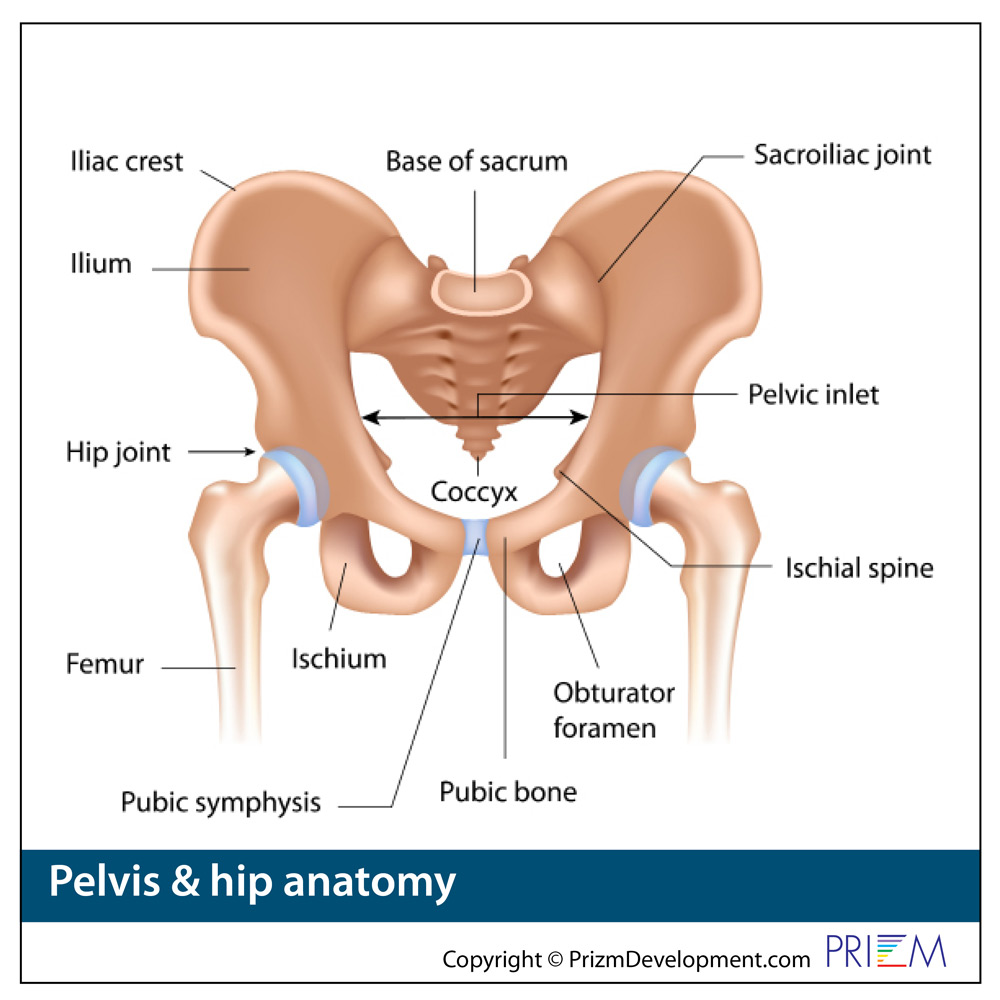 Hip
Hip
 Hip
Hip