Regenerative Medicine
 How new advances in Regenerative Medicine can relieve a variety of joint pain & orthopedic symptoms without surgery
How new advances in Regenerative Medicine can relieve a variety of joint pain & orthopedic symptoms without surgery
Do you have knee pain? If so you are not alone. Some estimates cite that 15% to 20% of all adult men suffer from knee pain, with incidence increasing with age and the onset of arthritis. Women may actually suffer worse from knee pain with almost one in four women experiencing knee pain.
About 800,000 total knee replacements and 544,000 hip replacements are done every year in the U.S., according to the American College of Rheumatology. This number continues to grow as our population ages.
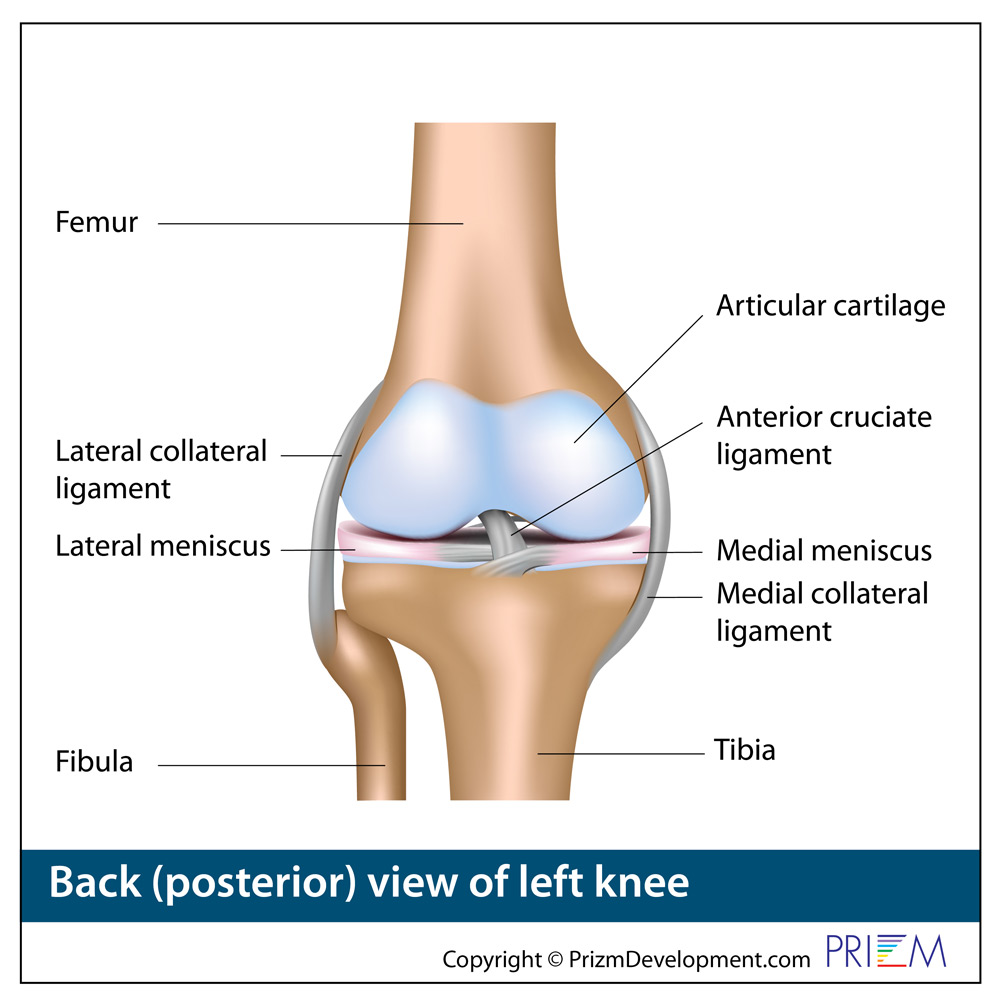
The growing number of joint replacements is tied to obesity. The human knee, for example, is an engineering masterpiece with four ligaments acting as guy wires to hold the knee joint stable and in position during running and jumping. But the human knee was not engineered to hold up a 300lb person.
Today in the United States, according to the National Institutes of Health, 44% of Americans age 40 to 69 are classified as obese. And that’s getting worse. The Centers for Disease Control (CDC) estimates that by 2030, half of Americans will be obese. For a 5’9” person, anything over 203 pounds would be obese.
Consequently, one of the first recommendations to relieve knee pain is to lose weight so the body is in a normal weight range to lessen the stress placed on the knee joint.
Thankfully, total joint replacement is one of the safest and most reliable joint replacement surgical procedures. Also advances in artificial joint technology can have a hip or knee implant last for 20 or more years before revision surgery is needed to replace it.
However, with that said, most orthopedic surgeons try to delay knee replacement surgery until the person is in their 50s, so they don’t outlive the lifespan of the joint and need that revision surgery, which can be complex to replace a worn out implant.
That means orthopedic surgeons often try to exhaust non-surgical treatment options for knee pain sufferers in the 20s to mid 50s.
REGENERATIVE MEDICINE: A new NON-surgical treatment option for musculoskeletal pain
Thankfully, for the educated healthcare consumer there is new hope with the emergence over the last 10 years of a new specialty called “regenerative medicine” which uses the body’s own healing properties to restore a knee or hip joint so that movement is less painful. The importance of this specialty is that it buys people time with their existing knee or hip joint so they are older when they consider major joint replacement surgery.
The regenerative medicine specialist harvests tissue or blood from a person’s own body, spins it down with a centrifuge and then injects the substance back into the arthritic joint the same day. This reduces inflammation from arthritis and can help the joint cartilage begin some level of healing. Within this are important living cells and growth factors that provide a healing function to damaged cartilage, tendons and meniscus.
The end result is that thousands of weekend athletes are back on their feet enjoying movement without pain — the same goal as surgical knee replacement but without the scalpel. The person is able to buy 10 or 20 years with regenerative medicine to reach that age where they have a good chance of outliving the lifespan of that artificial joint. The result is one joint replacement surgery rather than several risky re-do surgeries at an older age.
Buyer beware the charlatans
One of the problems, however, is that where there is a new medical advance, there is no shortage of charlatans that move in to exploit and take advantage of those who don’t do the necessary research to find the legitimate specialists in regenerative medicine.
To that end, the FDA in 2021 put out a warning that some unscrupulous clinics are bilking healthcare consumers under the tag of “regenerative medicine” when they are not providing any competence or specialization in that profession. The FDA warns that these charlatans are injecting dead stem cells harvested from other sources and charging patients exhorbitant fees for something that simply doesn’t relieve pain or provide any healing function to the joint.
Other countries have been more advanced in the use of stem cell therapy and providing helpful regenerative medicine for citizens while the FDA also has never approved a disease-modifying drug to provide relief from osteoarthritis.

There is huge demand currently in the U.S. for stem cell therapy and regenerative medicine when it is provided correctly, and FDA warning aside, that demand will continue as people try to regain movement in arthritic joints without solely depending upon a major joint replacement surgery.
There is now a growing number of respected regenerative medicine clinics and hospitals that offer stem-cell injections to relieve joint pain in a way the FDA agrees with: By extracting the body’s own bone marrow or fat, spinning it down in a centrifuge, and injecting it back the same day while the stem cells are still alive.
While the treatments are not yet covered by insurance, and the treatment can cost a few thousand dollars, thousands of these stem-cell patients have found that it works and they are back to activity without major surgery.
As with every medical advance, health insurance companies are the last to want to pay for a new treatment, new surgical implant, or procedure. It takes several years for an insurance company to realize that the non-surgical option saves them the cost of joint replacement and all the associated rehab costs post surgery. Consequently, it’s just a matter of time before regenerative medicine procedures are covered by insurance carriers.
Consequently, the burden is on the patient to search for a reputable regenerative medicine center that can provide a non-surgical solution to their damaged knee or hip joint while they buy time to delay the need for that surgical artificial knee or hip joint replacement.
Types of Regenerative Medicine
Rather than using outside drugs, or injecting outside substances, the concept of “Regenerative Medicine” is the umbrella term for advanced methods of reversing tissue damage and REGENERATING the body by using the body’s OWN HEALING SUBSTANCES.
The term “stem cell” has varied connotations. Related to orthopedics, stem cell treatment is essentially using what cells are already in your own body, only increasing the effectiveness of your own cells.
Why a person might explore regenerative medicine and stem cell treatment over knee replacement surgery?
Regenerative Medicine
New non-surgical treatment options are available to relieve joint pain symptoms, and potentially delay joint replacement surgery until later in life when they are less likely to outlive the lifespan of an artificial joint. Regenerative medicine therapies have shown great promise in treating many conditions outside of joint pain, as you are using the body’s own healing powers, but simply strengthening these natural healing systems.
Physicians can use Platelet Rich Plasma, cellular-based therapies, and alpha 2 macroglobulin for regenerative medicine treatments. They are trained to harvest and inject adipose-derived cells and bone marrow aspirate to speed the body’s own healing capabilities.

Where do stem cells come from?
Most orthopedic physicians use cellular-based therapies to accelerate the body’s natural healing systems. This can include harvesting specific cells from the patient’s own body — from either their bone marrow or from their fat cells. While early research focused on the cells found in birth tissues, these types of cells are not typically used in an orthopedic setting.
If you are considering regenerative medicine and cellular-based therapy, be sure to ask your physician what source of stem cells they plan on using.
Regenerative Medicine & Cellular-based Therapies
Rather than using outside drugs, or injecting outside substances, the concept of “Regenerative Medicine” is the umbrella term for advanced methods of reversing tissue damage and REGENERATING the body by using the body’s OWN HEALING SUBSTANCES.
Related to orthopedics, mesenchymal signaling cells (MSCs) and “cellular-based therapy” treatment is essentially using what cells are already in your own body, only increasing the effectiveness of your own cells.
About Alpha 2 macroglobulin for relief of pain from arthritis
A Florida-based research company, Cytonics, has developed a method for injecting Alpha-2-macroglobulin, or A2M, to stop the progression of arthritis. According to the Cytonics, the injections inhibit the progression of arthritis and arthritic joints, and can regenerate damaged cartilage in affected joints.
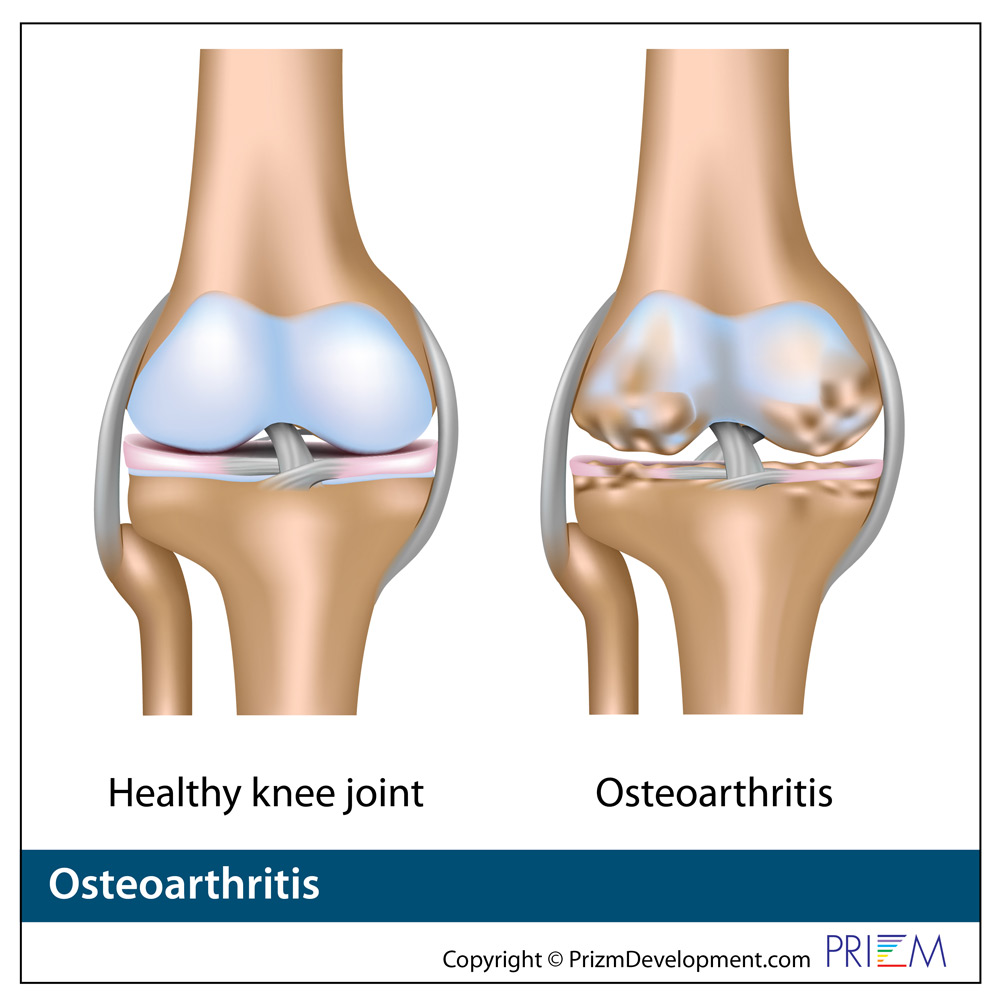
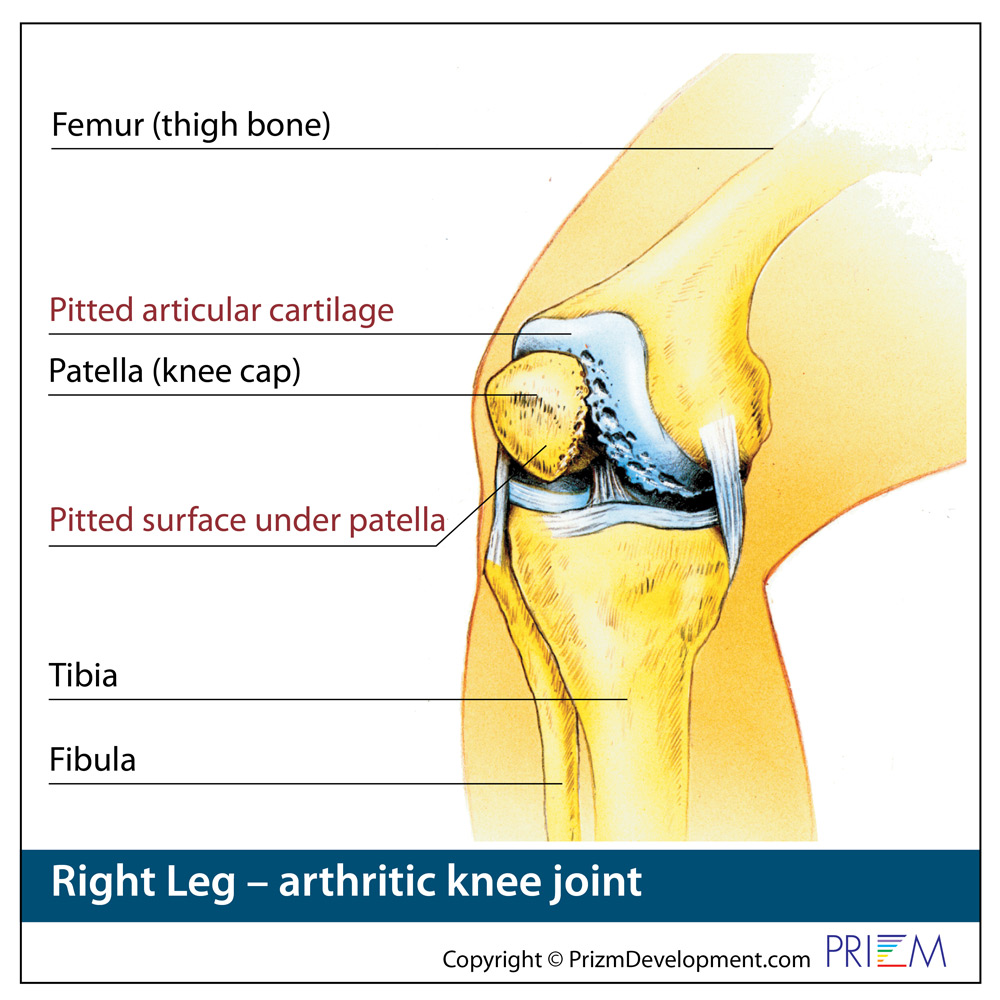
When a patient has arthritis, chemicals cause cartilage to break down causing joint pain and inflammation. Over several years, these chemicals involved in the disease of arthritis can cause the cartilage to disappear completely. This causes painful bone-on-bone friction. In healthy joints, convesely, the healthy cartilage works as a buffer to prevent bone-on-bone contact.
A2M halts the progression of osteoarthritis at the molecular level by inactivating the chemicals that cause the joints to breakdown. As the A2M captures and neutralizes the damaging chemicals, the body works to eliminate them. The joint will then begin to recover, as the inflammation is subdued, and harmful chemicals are no longer present. A2M remaining in the joint will promote tissue growth and the joint can begin the restoration process. The repaired damage will then lead to a pain-free joint.
This A2M joint treatment works best when used early in the onset of arthritis before the chemicals associated with arthritis have destroyed the cartilage and the joint. Early intervention saves the maximum amount of cartilage in the joint.
In those with longer-stage untreated arthritis, A2M injections may still be effective. The restoration process may not be as dramatic, but will still inhibit disease progression.
About bone marrow aspirate
Bone marrow aspirate contain stem cells, platelets and growth factors obtained from your own bone marrow. Bone marrow is the tissue that is found in the center of bones responsible for creating blood cells. For regenerative medicine, the bone marrow aspirate would be harvested from a person’s own hip or pelvic bone.
Bone marrow was the first body tissue used to obtain stem cells. While harvesting bone marrow from the patient’s own body eliminates the risk of rejection and increases the likelihood the body will benefit from the injection, bone marrow stem cells may not be as concentrated and may be less likely to multiply and specialize compared to stem cells harvested from the patient’s own adipose tissue.
Platelet Rich Plasma (PRP) Therapy for Joint and Tendonitis Pain
Plasma is the clear portion of the blood in which all the other blood components – platelets, red blood cells and white blood cells – travel. Each blood component has a different job.
Platelets have the ability to recognize damaged blood vessels. When you have a cut, platelets are drawn to the injured area where they begin to stick together to form a plug to stop the bleeding. As these platelets group together, they begin to change their shape from a disc to a spiny octopus like structure, entangling more and more platelets. These platelets, along with other proteins released within the body create a hard scab which completely stops the bleeding and protects the injury while it heals. A similar process occurs inside the body when you have a broken bone or injury that bleeds internally.

These platelets contain natural growth hormones and proteins that tell your tissues to increase rebuilding to enhance your recovery and help stop pain symptoms.
Platelet rich plasma, commonly referred to as PRP, is the patient’s own human blood that is spun down in a centrifuge and separated producing a concentration of platelets above the natural values commonly found in their blood. Platelet rich plasma can have as much as eight times more than the normal amount of platelets. This concentration of platelets from the patient’s own blood is then collected and injected back into the person at the site of injury.
The goal of PRP therapy is to enhance the body’s natural ability to repair itself to speed healing and shorten recovery time from muscle, ligament, tendon and joint injuries. PRP can be especially helpful for long-standing chronic injuries that have taken a long time to heal. Injecting concentrated platelets at the site of injury can accelerate the body’s own healing response.
PRP has been used in a variety of fields over the years, including plastic surgery, sports medicine and dermatology. Some prominent professional athletes have received PRP, including golfing great Tiger Woods and tennis champion Rafael Nadal.
There are some conflicting studies about the value of PRP, and which type of centrifuges may produce the optimal plasma. No studies to date have documented any adverse effects associated with PRP. So in that sense, there is no downside to the therapy. Because the injected platelets are produced from a person’s own body, there typically is no issue related to rejection or transmitting disease.
How is PRP administered?
A person undergoes PRP therapy in the physician’s office. The patient is instructed to stop all anti-inflammatory medication or steroids at least one week beforehand as these medications negatively affect platelets.
A small amount of blood are drawn from the patient’s arm. This blood sample is then placed into a centrifuge which spins the blood down so the heavier parts sinks to the bottom. Platelets and white blood cells spin out above this bottom layer and these concentrated platelets are collected and used for the injection.
PRP typically only requires local numbing medication at the injection site. No general anesthesia or sedation is required.
When to expect relief?
PRP does not provide instantaneous relief from symptoms. Growing new tissue and healing injured joints can take one to three months. But for those people who have seen their healing process stall, PRP can jumpstart the body’s own healing process.
There is great variability in the success of PRP based on the experience of the physician specializing in PRP, the type of centrifuge used, and selection of the ideal patient who can benefit from PRP.
Stem Cell Therapy for Knee Pain

The term “stem cell” has received a bad reputation over the years, largely due to research involving human embryos and the misperception that all stem cells come from embryos or amniotic tissues.
But, a stem cell is simply a type of cell that already exists in your body that has the unique ability to produce other cells, become a different kind of cell, or instruct other cells how to behave based on the task the body requires.
All other cells in the body are created for a specific purpose. For example, a red blood cell has the job of transporting oxygen throughout the body. But, that red blood cell is not able to divide and reproduce. Instead, when the body requires new red blood cells, it is the job of the stem cells located in your bone marrow to produce the new red blood cells. Those same stem cells can also produce white blood cells and platelets.
Stem cell therapy is the process of delivering these unspecialized stem cells to a targeted location in your body to stimulate new cell growth and tissue healing. When stem cells are injected into an arthritic joint or injured tendon or ligament, they attach to the areas of damaged tissue to initiate the healing process.
How is stem cell therapy performed?
Stem cell therapy is typically performed in the office. If the physician is sourcing the stem cells from adipose (fat) tissue, the treatment will begin with liposuction to remove fat from the patient’s own belly region or buttocks. Only a small amount of tissue is harvested, so there will be no cosmetic difference to the liposuctioned area. Bone marrow aspirate can also be used because it contains stem cells, platelets and growth factors.
This collected fat tissue is processed in the office lab so the portion of the harvested tissue that contains the stem cells can be collected.
Next the physician injects the concentrated sample of stem cells into the damaged joint or tendon. The stem cells then work directly at the site of injury, or on degenerative tissue to greatly accelerate the natural healing process.
In a sense, stem cell treatment is essentially using the body’s own natural healing properties, but condensing it into a stronger dose and applying it to the body’s injured site to accelerate healing.
Stem Cell studies show promising results
While stem cells over the last 10 years stimulated a wide debate, the reality is that the therapy has become very mainstream, and is used by many professional athletes to accelerate healing so they can return to their sport.
For example, researchers at the Mayo Clinic conducted the world’s first prospective, blinded and placebo-controlled clinical study to test the benefit of using bone marrow stem cells for arthritic knee pain. It is the first time stem cells have been tested in such a rigorous fashion. The findings in The American Journal of Sports Medicine found that patients not only had a dramatic improvement in the knee that received stem cells, but also in their other knee, which also had painful arthritis but received only a saline control injection. Each of the 25 patients enrolled in the study had two bad knees, but did not know which knee received the stem cells.
A recent study showed that stem cell therapy for knee arthritis resulted in a 58-68% improvement in pain and 67-83% improvement in function one to two years after treatment. One study from 2014 showed that stem cell injections given after surgery to remove torn knee cartilage showed evidence of cartilage regeneration and lessened pain.
Are there any side effects or risks from stem cell treatment for knee pain?
Stem cell treatment for knees is noninvasive, and studies suggest that side effects are minimal. After the procedure, some people may experience temporary increased pain and swelling. However, the overwhelming majority of people who get stem cell injections have no adverse side effects.
The method where stem cells are harvested from your own body, dramatically reduces the risk of any serious side effects. However, there are various ways of harvesting and processing the stem cells, which likely affects the various success rates of the published studies.
Again, before receiving any stem cell treatment, it’s best to learn as much as you can about the physician and the stem cells they are using. There can be wide variation in success based on the physician and how experienced they are with stem cell treatment of knee pain.

 Knee
Knee
 Knee
Knee
 Knee
Knee
